Colonoscopy
A colonoscopy is considered the gold standard in colorectal cancer screening. It allows doctor to both examine the colon and rectum and remove polyps (growths that can turn into cancer) in the same procedure.
What happens during a a colonoscopy?
- During a colonoscopy, your doctor will give you a light sedative to help you stay relaxed.
- The doctor will then insert a long, flexible, lighted tube with a camera called a colonoscope into the anus and slowly guide it through the rectum and into the colon. The scope inflates the large intestine with carbon dioxide gas to give the doctor a better view.
- The camera on the scope transmits a video image from inside the large intestine to a computer screen, which allows the doctor to carefully examine the intestinal lining.
- The doctor will examine the entire colon searching for anything abnormal. If present, polyps (growths in the lining of the colon that can turn into cancer) are removed.
- Once the scope has reached the opening to the small intestine, it is slowly withdrawn and the lining of the large intestine is carefully examined again.

The colonoscopy prep
Your doctor will give you specific directions on how to prep for your colonoscopy. Generally, all solids must be emptied from the stomach and bowel with laxatives and a clear liquid diet.

Colonoscopy pros
- Most thorough screening method available
- Allows doctor to both examine the colon and remove polyps (growths that can turn into cancer) in the same procedure
- Sedation is usually given to patient to minimize discomfort
- Examines full colon
- Depending on results, may only need to be re-screened every 10 years

Colonoscopy cons
- Requires one day of clear liquids and laxative preparation
- Will need to set aside a day for the procedure
- Will need to have a ride home to leave the medical facility
- Very slight risk of perforation or bleeding
Learn more
Are colonoscopies dangerous?Top resources

Legislation introduced to address young-onset CRC
Explore the urgent need for the Colorectal Cancer Early Detection Act (HR 7714), legislation aimed at combating the rising incidence of colorectal cancer among younger adults through enhanced screening, education, and research.
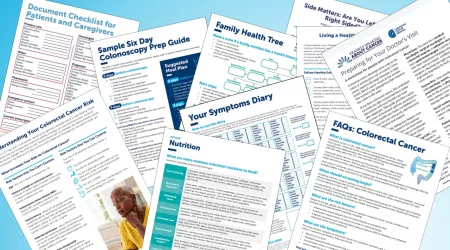
Colorectal cancer resources for learning and sharing
Whether personally impacted by colorectal cancer (CRC), supporting a loved one, or dedicated to educating and empowering others, these downloadable and printable resources can help.

Dak Prescott joins Alliance to ‘LEAD FROM BEHIND’
Initiative aims to reduce stigma and educate about screening choices, as the Colorectal Cancer Alliance launches a health equity fund to decrease disparities.





