Stage III

What is stage III colorectal cancer?
Stage III colorectal cancer has spread into nearby lymph nodes, but has not reached other areas of the body.
Colon cancer
Stage III colon cancer is divided into three categories.

Treatment for stage III colon cancer
The standard treatment for stage III colon cancer is:
- Surgery to remove the section of the colon that has cancer (partial colectomy). Your surgeon will also remove nearby lymph nodes during this procedure.
- Chemotherapy:
Most often the FOLFOX (5-FU, leucovorin, and oxaliplatin) or CapeOx (capecitabine and oxaliplatin) regimens are used.

Radiation therapy for stage III colon cancer
Stage III colon cancer that cannot be removed completely by surgery may be treated with chemotherapy along withradiation therapy to shrink the cancer so it can be removed later with surgery.
Radiation therapy may also be used for stage III cancer after surgery because:
- The cancer was attached to a nearby organ.
or
- The tissue that was removed had positive margins (cancer was found in the edges of the area left behind).
Rectal cancer
Stage III rectal cancer is divided into three categories.
Treatment for stage III rectal cancer
Stage III rectal cancer is usually treated with a combination of:
Chemotherapy
Radiation therapy
Surgery
Every person's diagnosis is different, so the order of these three treatments may vary.
Chemo & radiation
In most cases chemotherapy (usually 5-FU or capecitabine) and radiation are the first treatment. This allows the tumor to shrink in size before surgical treatment.
Surgery
Surgery is usually the second phase. Depending on where the the cancer is located in the rectum, surgeries that may be performed are:
Abdominoperineal resection (APR)
If the cancer has spread to nearby organs, a surgery called pelvic exenteration may be needed.
Additional chemo
The third phase is additional chemo after surgery.
Chemo drugs may be:
FOLFOX regimen (oxaliplatin, 5-FU, and leucovorin)
5-FU and leucovorin
CAPEOX (capecitabine plus oxaliplatin)
Capecitabine alone
Colorectal cancer stages
Stage IVTop resources

Christy Williams: Biomarker testing leads to successful treatment
Statistics suggested that Christy’s odds of survival were grim, so she leaned into her faith and kept a positive outlook. She tried to control what she could. And, critically, she received biomarker testing.
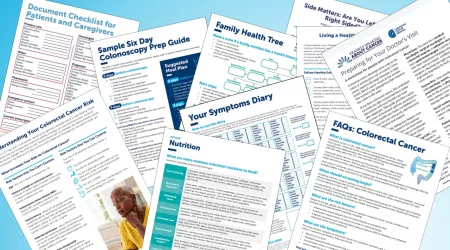
Colorectal cancer resources for learning and sharing
Whether personally impacted by colorectal cancer (CRC), supporting a loved one, or dedicated to educating and empowering others, these downloadable and printable resources can help.

Don Shippey: from stage IV to six years cancer-free after receiving HAI pump
Don Shippey was 55 years old in 2016 when he decided he’d been putting off his colonoscopy long enough.





