Lynch syndrome
Lynch syndrome is an inherited condition that greatly increases a person’s risk for developing colorectal cancer. It is the most common inherited form of colorectal cancer.
The facts
- Three to five percent of all colorectal cancer patients are diagnosed with Lynch syndrome.
- About one in 300 people have a harmful genetic mutation in their DNA that causes Lynch syndrome.
- The average age of onset of colon cancer in Lynch syndrome patients is between 40-60, while the average age in sporadic (random) patients is between 67-71.
- When one parent has Lynch syndrome, each child has a 50% chance of having Lynch syndrome.
- Lynch syndrome increases the risk for several other types of cancer, including endometrial cancer (uterine cancer), ovarian cancer, gastric (stomach) cancer and other types of cancer.
Causes, risks, prediction, and diagnosis
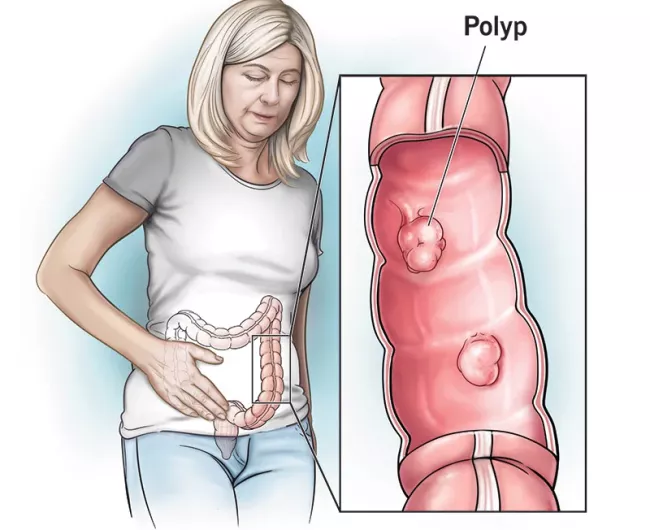
Polyps with Lynch syndrome
- If a polyp is found, it should be removed by endoscopy.
- If a polyp cannot be removed by endoscopy, discuss with your doctor the surgical options best suited for you.
- If an advanced polyp is found during your colonoscopy, discuss with your doctor the different surgical options most suited for you.
- It is common for people with Lynch syndrome to have flat polyps that can be difficult to detect. Talk to your doctor about screening for these.

Treatment options for Lynch syndrome
Lynch syndrome patients with colon cancer are treated similarly to colon cancer patients without Lynch syndrome.
Depending on the stage of diagnosis, a typical treatment plan will include surgery, chemotherapy, and immunotherapy.
Lynch syndrome and cancer screening
People with Lynch syndrome should get screened early and often. Talk with your doctor about a screening plan to reduce your risk of developing colorectal or other cancers.
Early screening saves lives
Start at the age of 20-25, or two to five years younger than the youngest relative who was diagnosed with colorectal cancer.
Screen often
Continue with colonoscopy every one to two years until the age of 40, even if no polyps or pre-cancerous growths are found. Make sure to get a colonoscopy every year after 40.

Other things to consider
- Plan for annual total body skin exams, since skin cancer is associated with Lynch syndrome.
- Some studies have shown that daily aspirin may reduce the risk of developing colorectal cancer and other types of cancer in people with Lynch syndrome. Ask your doctor before taking any new medication.
- Some people with Lynch syndrome may consider surgically removing their whole colon (prophylactic colectomy), even before cancer is detected, to reduce the risk of developing colorectal cancer.

Women & Lynch syndrome
Women with Lynch syndrome should have a screening plan for endometrial cancer and ovarian cancer that includes an annual:
- Transvaginal ultrasound
- Blood test for the CA125 biomarker
Consider having surgery to remove your uterus (hysterectomy) and ovaries (oophorectomy) to reduce risk of endometrial and ovarian cancers.
Other inherited conditions
FAP syndromeTop resources
Colorectal cancer resources for learning and sharing
Whether personally impacted by colorectal cancer (CRC), supporting a loved one, or dedicated to educating and empowering others, these downloadable and printable resources can help.

Michelle Cappel: Biomarker testing extends life
Michelle Cappel owes a lot to colorectal cancer biomarker testing — seven years of life and counting.

Not all states mandate biomarker testing coverage
While Congress has yet to bring Medicare coverage fully up to speed with advances in biomarker testing, many states are acting.





