Stage IV
What is stage IV colorectal cancer?
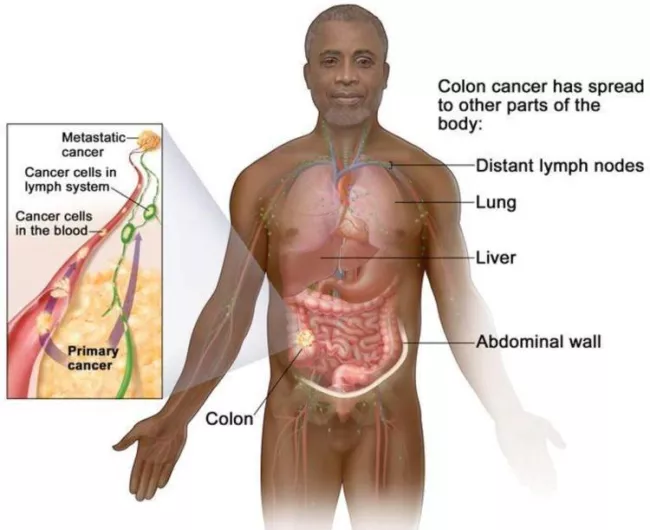
In stage IV (metastatic) colorectal cancer, the cancer has been carried through the lymph and blood systems to distant parts of the body. The most likely organs to develop metastasis from colorectal cancer are the lungs and liver.
Colon cancer
Stage IV colon cancer is divided into three categories.
Rectal cancer
Stage IV rectal cancer is divided into three categories.

Treatment for stage IV colorectal cancer
Stage IV colorectal cancer treatment may include any of the following:
- Surgery to remove or reduce the size of the cancer in the colon or rectum, or to remove cancer that has grown on other organs, such as the liver, lungs, prostate, or ovaries.
- Radiation or chemotherapyto relieve symptoms as part of palliative care.
- Targeted therapy
- Immunotherapy
- Clinical trials
Cancer that has spread to the liver
The liver is the most common site of metastasis in patients with colorectal cancer, due to the blood supply that exists between the large intestine and the liver.
There are a number of therapies that use chemotherapy, ablation, radiation,cryotherapy, and other approaches to reduce or remove liver metastases.
Many of these therapies are minimally invasive and have a short recovery time.
First steps
A stage IV (metastatic) colorectal cancer diagnosis can leave you with many questions. Here are some first steps to consider.
Top ten questions to ask your doctor
Some guidelines for the right questions as a newly diagnosed patient.
Explore clinical trials
Finding a clinical trial can be intimidating, but we are here to help you explore your options and help you prepare a list of trials to take to your doctor.
Sign up for BlueHQ
BlueHQ is your free support hub with direct access to the Alliance’s universe of tools, resources, and peer communities.
Your emotional health
Just as cancer affects your physical health, it can bring up a wide range of emotions you’ve never faced before.
Clinical trials: where do you start?
Try our clinical trial finderTop resources
Colorectal cancer resources for learning and sharing
Whether personally impacted by colorectal cancer (CRC), supporting a loved one, or dedicated to educating and empowering others, these downloadable and printable resources can help.

Don Shippey: from stage IV to six years cancer-free after receiving HAI pump
Don Shippey was 55 years old in 2016 when he decided he’d been putting off his colonoscopy long enough.
Gabriel Leblanc: How the Alliance changed my life
It’s scary to hear the “c” word, especially when you’re only 36. A million questions ran through Gabriel Leblanc’s mind, but only one seemed to matter. “How was I going to get through this?” Gabriel said.





